Many aspects of the system need change now
By Matthew Fraser, Opinions Editor
There is a certain optimistic hope that we are past the worst of what may be the first run of COVID-19; it’s now time to begin to consider the lessons learned and future actions needed to prevent another massive economic and health care disaster. From one end of the country to the other, a light was shone on the current state of our health care system; though it is never far from us, it is often overlooked in our day-to-day existence. However, as personal protective equipment (PPE) ran low or out around the country with no foreseeable replenishments, the nation was forced to an unfortunate reckoning. And, as some long-term care centres around the country lost their patients in swathes and their ability to cope, another hole in our system was ripped open. What deficiencies can be solved soon to prevent a repetition of this abysmal state?
One of the worst things a graduate could face as they leave their school is an assurance that they will not have a job. Worse still would be if that job was one they had spent the past ten years training for. This exact situation faces hundreds of Canadian medical school graduates who do not have residencies at the time that they finish school. The issue is so bad that groups like the Canadian Federation of Medical Students have fallen to lobbying the government to increase their prospects in order to combat the year after year increase in unmatched graduates. Of the many things we have learned during this pandemic, we should see that these unmatched students are wasted resources. As if that wasn’t bad enough, citizens trained outside of Canada have resorted to suing the government in order to get residencies as well (granted this preference exists so that Canadian school graduates don’t end up unemployed). All this before we speak about foreign trained and certified immigrants unable to practice as nurses, doctors, and other medical professionals.
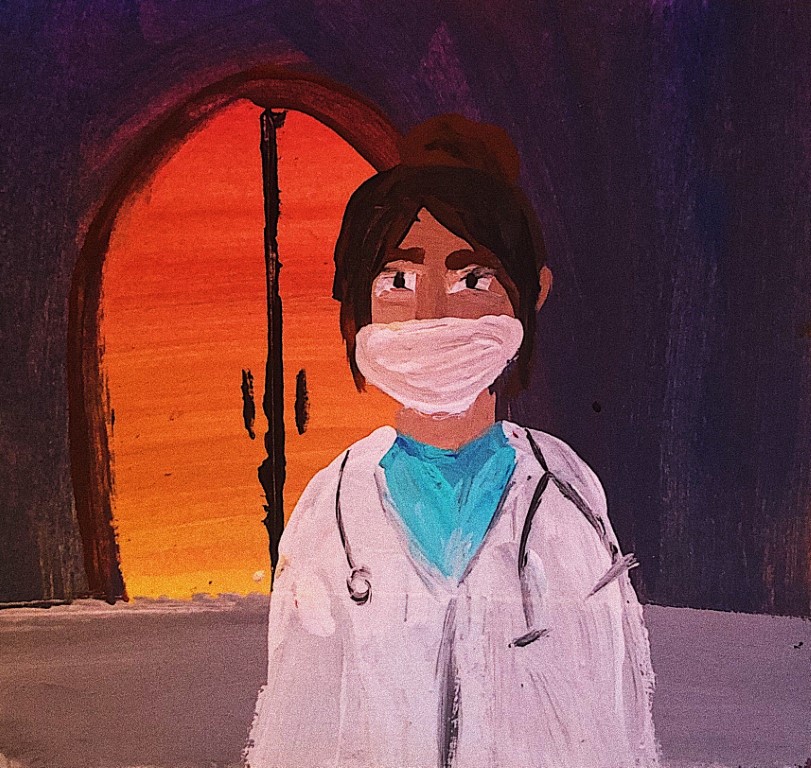
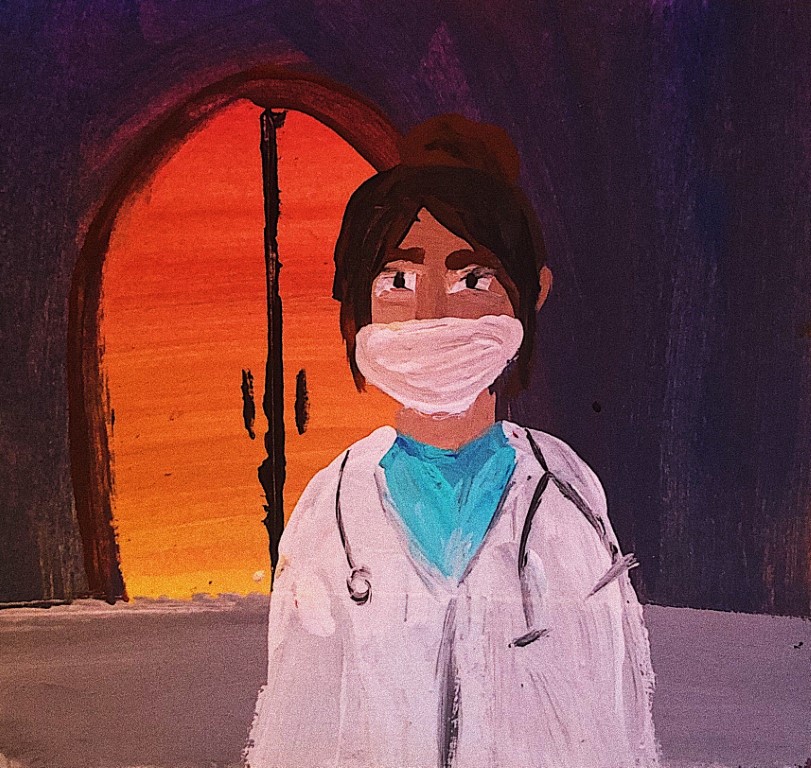
For the doctors and nurses trained and working in the field, there comes a new and potentially more horrendous situation: the possibility of a PPE famine. As detailed in a National Post article, some health care professionals are concerned about the chance of a supply shortages and being unprotected. Though the federal government has placed orders for millions of dollars worth of equipment, the fact that this is not a situation unique to Canada and is unsettling.
Heartbreaking pictures of the extreme isolation that many care homes have been forced to mandate have filled the news. But with these pictures come with shocking tales of long-term care homes with COVID-19 positive patients. For reference, a new study published in The Star states that 82 percent of all Canadian COVID-19 deaths come from elderly in long-term care. As of May 6, 3,436 care home residents had died of COVID-19—making up a huge chunk of the 4,167 Canadians who have passed due to coronavirus. We are now forced to see how the warehousing of the elderly has continued to fail some of the most vulnerable.
The pandemic may continue to plague us in the years to come, but Canadians must begin to look at the steps necessary to fortify us against future epidemics. If that means allowing students to complete their residencies outside of Canada and prioritizing moving immigrants with medical degrees into more suitable careers, now is the time to begin that debate. If emergency production laws need to be reconsidered and PPE manufacturing increased in the nation, it is clear that it can only help us in the future; with the rapidly aging Canadian population, there’s no doubt that safety in care centres needs to be improved. Hopefully as a country we can change these things before it is once again too late.